Head and Neck Squamous Cell Carcinoma (HNSCC) is a highly complex and aggressive form of cancer that arises from the mucosal surfaces of the head and neck. Despite advancements in treatment, its prognosis remains challenging due to the intricate interplay between genetic mutations, tumor microenvironment, and immune responses.
Genetic Landscape of HNSCC
HNSCC is driven by various genetic alterations, including mutations in TP53, CDKN2A, and NOTCH1. These mutations disrupt crucial cellular functions such as DNA repair, cell cycle regulation, and differentiation, leading to uncontrolled tumor growth. Additionally, human papillomavirus (HPV)-associated HNSCC presents a distinct mutational profile, which has implications for prognosis and treatment strategies.
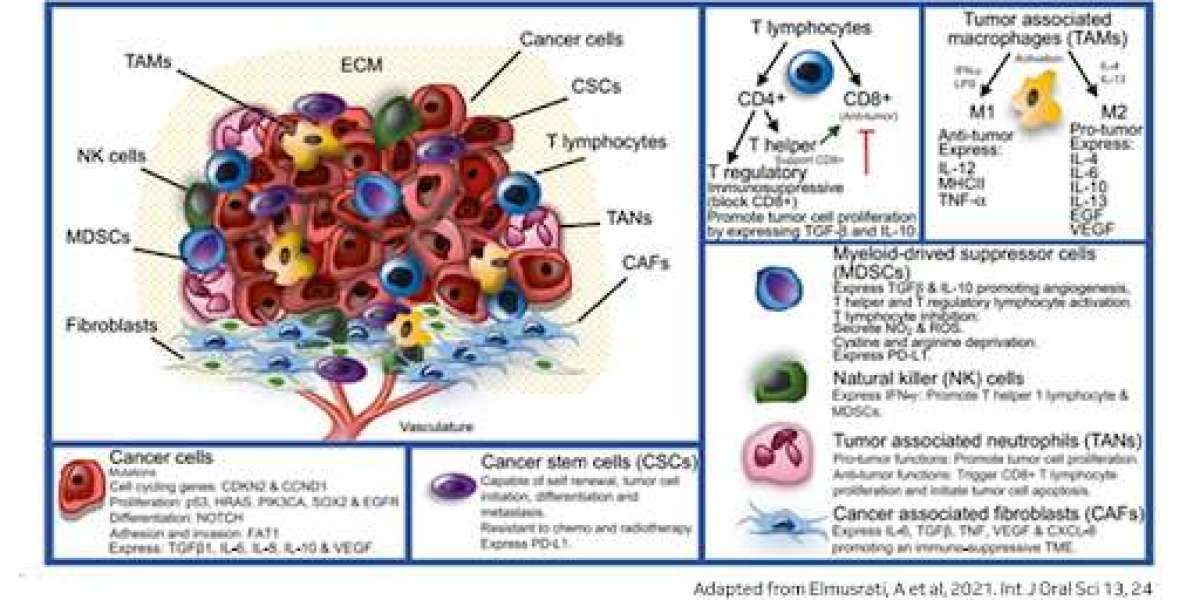
The Role of the Tumor Microenvironment
The tumor microenvironment (TME) in HNSCC is composed of immune cells, stromal components, and signaling molecules that influence tumor progression and resistance to therapy. Immune evasion mechanisms, such as the overexpression of immune checkpoint proteins (e.g., PD-L1), allow tumors to escape immune surveillance, making immunotherapy an emerging avenue for treatment.
Therapeutic Implications
Understanding the molecular and microenvironmental factors driving HNSCC has paved the way for targeted therapies, including EGFR inhibitors, immune checkpoint inhibitors, and personalized treatment strategies based on molecular profiling. Ongoing research aims to identify novel biomarkers and combination therapies that can improve patient outcomes.
Conclusion
HNSCC is a multifaceted disease that requires a comprehensive approach, integrating genomic insights and tumor microenvironment studies. Advancements in precision medicine hold promise for more effective and personalized treatment strategies, ultimately improving survival rates and quality of life for patients.
For an in-depth exploration of the latest research on HNSCC, visit the full blog at MedGenome Research.