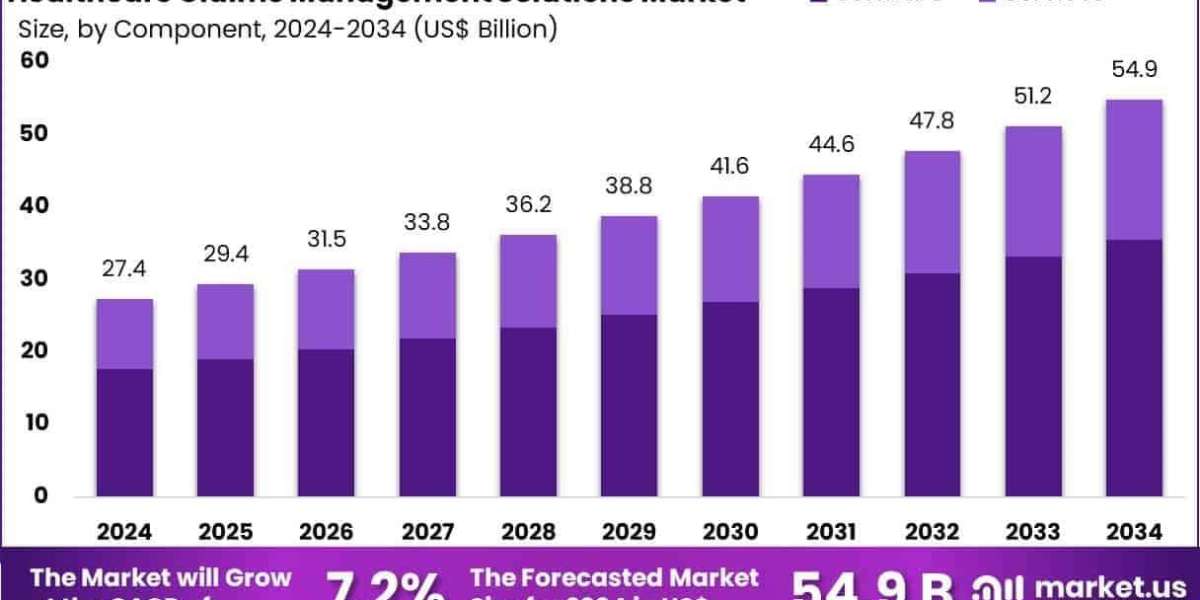
The Global Healthcare Claims Management Solutions Market Size is expected to be worth around US$ 54.9 Billion by 2034, from US$ 27.4 Billion in 2024, growing at a CAGR of 7.2% during the forecast period from 2025 to 2034. North America held a dominant market position, capturing more than a 38.2% share and holds US$ 10.4 Billion market value for the year.
The Healthcare Claims Management Solutions Market is undergoing a major overhaul in 2025, propelled by AI-driven automation and data analytics. Health plans and providers are deploying intelligent claims platforms that can instantly flag errors, predict denials, and automate resubmissions, reducing manual intervention. These advanced solutions are lowering administrative costs while accelerating reimbursement cycles.
Vendors are incorporating predictive insights into risk scoring and fraud detection. As healthcare systems embrace value-based care, claims data is being leveraged for network optimization and cost transparency. With regulatory pressure to reduce overpayments and streamline billing, AI‑powered claims tools are becoming essential in the U.S. healthcare ecosystem.
Click here for more information: https://market.us/report/healthcare-claims-management-solutions-market/
Emerging Trends
- AI-based denial prediction: Machine learning models analyze past claim trends to anticipate high-risk submissions and suggest preemptive corrections.
- Integrated fraud analytics: Claims platforms now cross-reference provider behavior, regional trends, and utilization data to detect anomalies.
- Real-time patient eligibility checks: Systems automatically validate coverage and benefits before services are rendered to avoid downstream denials.
- Value‑based claim scoring: Solutions assign quality metrics and outcome-based scores to claims, enabling better provider benchmarking.
Use Cases
- A payor uses an AI tool to process 10,000 claims daily, reducing manual review time by 60%.
- A hospital leverages fraud analytics to audit high-cost claims, recovering millions in avoidable payments.
- A multi-state practice integrates real-time eligibility checks in its billing system, cutting denial rates by 25%.
- An accountable care organization applies outcome-based scoring to prioritize high-value providers in their network.