How Medical Billing Works in Mental Health Care
Mental health care is crucial for overall well-being. So, paying for these services can be confusing. Whether you are a patient in therapy or a provider, understanding medical billing in mental health is crucial. Medical billing goes beyond just sending an invoice. It is a detailed, multi-step process that links healthcare providers with insurance companies. This system ensures that services are reimbursed correctly. when we did it in right way this helps providers to reduce their financial stress for patients. However, if it’s misunderstood or mishandled, it can lead to delays, denied claims, and unexpected costs.
In this article, we will look at the step-by-step process of mental health billing. We will also discuss how it differs from general medical billing and why it matters for both clients and clinicians.
The Basics of Medical Billing in Mental Health
Mental health billing begins when a patient books an appointment with a licensed provider. This can be a psychologist, psychiatrist, counsellor, or therapist. In Health care, mental health services usually require ongoing sessions. This can make the billing process more frequent and sometimes more complex.
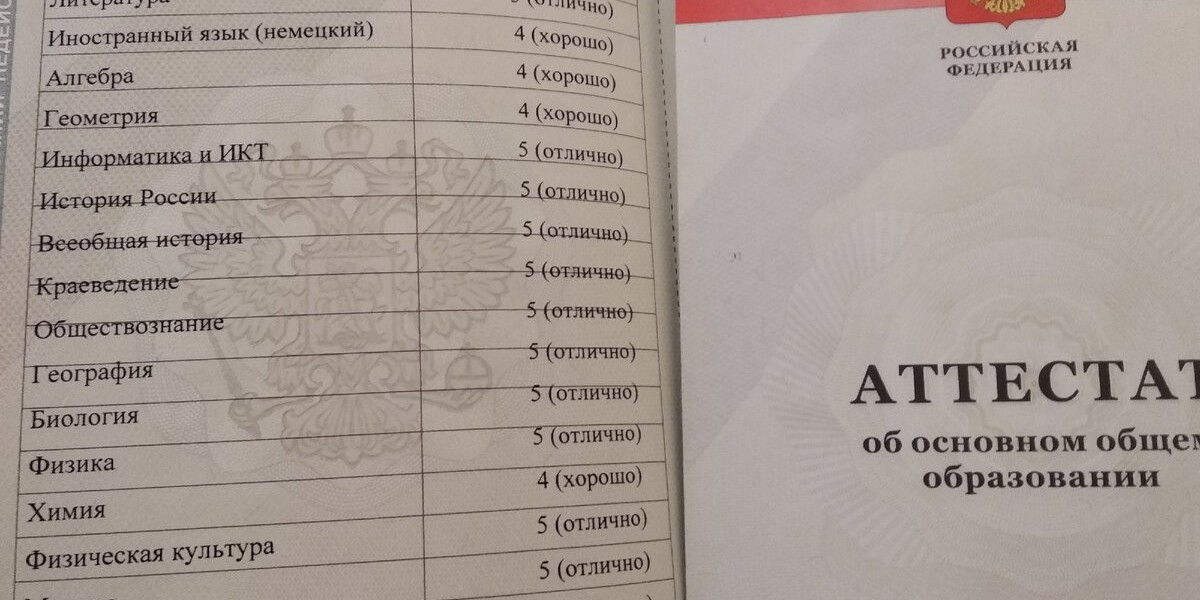
Once the session is completed, the provider (or their billing staff) creates a superbill or claim that includes:
Patient details (name, insurance, date of birth)
Diagnosis codes (ICD-10)
Procedure codes (CPT codes)
Session duration and provider details
This information goes to the patient’s insurance company, either directly or via a clearinghouse. Then, the insurance company reviews the claim. They decide how much to cover based on the patient’s plan, deductible, and network requirements. After approval, the insurance company pays part of the cost to the provider.
Challenges in Mental Health Billing
Unlike billing for a broken arm or a blood test, mental health services have layers of nuance. A few challenges include:
Authorization requirements: Some insurance plans require prior approval before therapy begins.
Session limits: Policies may only cover a certain number of sessions per year.
Confidentiality and stigma: Patients may be hesitant to share sensitive information with insurers.
Coding complexity: Therapists must pick the correct CPT codes for sessions, like 90834 or 90837. Errors can lead to denials.
Also, mental health professionals handle many roles. They provide care, manage records, and deal with admin tasks. This makes outsourcing billing a common choice.
A Closer Look: The Role of ABA Billing Services
As mental health care grows to include therapies like Applied Behavior Analysis (ABA), billing gets more complex. ABA therapy helps individuals with autism spectrum characteristics (ASC) and conforms to particular rules, codes, and insurance guidelines.
This is where ABA billing services come in. They manage prior authorizations and submit claims with correct CPT and modifier codes. They help patients to get money at the right time. They also ensure families avoid unexpected billing problems.
Partnering with a billing specialist lets ABA providers focus on care. They no longer need to track denials or chase payments. This benefits both therapists and families who rely on consistent support and timely sessions.
The Medical Billing Lifecycle: Step-by-Step
To fully understand how mental health billing functions, it’s helpful to walk through the entire billing lifecycle:
1. Patient Intake & Insurance Verification
When a client first reaches out to a mental health provider, the intake process begins with collecting insurance information. Verification checks if the patient’s plan covers mental health services. It also identifies copayments, deductibles, and whether the provider is in-network or out-of-network.
2. Service Documentation
After each session, the therapist writes down details of the visit. They make a report about the therapy they used and how much time spent. This process ensures accurate coding and helps justify claims if an insurance company asks for more information.
3. Coding & Claim Submission
The provider assigns CPT codes, such as 90832 for a 30-minute therapy session and 90837 for 60 minutes. They also assign diagnosis codes. These codes are sent through billing software or clearinghouses to the payer, which is the insurance.
4. Claim Scrubbing & Adjudication
Claims are checked for errors before being processed. If clean, they move into adjudication—where the insurer decides if the service is covered and at what rate.
5. Payment or Denial
If approved, the insurer sends an Explanation of Benefits (EOB) and payment. If denied, the claim may require corrections or appeals. Patients are then billed for any remaining balances.
6. Appeals & Resubmission (if needed)
Denied or underpaid claims can be appealed. Skilled billers know how to write compelling appeals and fix errors that may have led to the rejection.
In-Network vs Out-of-Network Billing
Mental health providers can be in-network or out-of-network. In-network providers have contracts with ABA Credentialing services kind of insurance companies. They agree to set rates, which often lowers costs for patients. However, this means more paperwork for providers.
Out-of-network providers can set their own rates. Patients may pay more upfront and need to file their own claims. It’s important for clients and clinicians to understand these trade-offs when beginning a therapeutic relationship.
Technology and the Future of Mental Health Billing
Telehealth and digital health records are making billing easier. However, they also rely more on automation and compliance. Software tools assist with scheduling, eligibility checks, claim submission, and reporting.
AI-driven billing platforms are now here. They use predictive analytics to spot potential denials early. These tools help solo practitioners and large therapy groups by cutting revenue loss and reducing administrative work.
Providers must also stay alert about data privacy, especially with sensitive mental health records. HIPAA compliance and secure data handling are crucial.
Why This Matters to You
If you’re a patient, knowing how billing works helps you avoid surprise costs. It also prepares you to ask the right questions during therapy onboarding. If you’re a provider, especially in mental health, understanding billing is key. Partnering with experts can also ensure you get paid on time and keep your practice sustainable.
Accurate billing supports better access to care. When providers are reimbursed fairly and promptly, they’re better equipped to serve more clients and reduce waitlists.
Final Thoughts
Mental health billing may not be glamorous, but it’s a crucial part of the therapeutic ecosystem. Whether it’s verifying benefits, selecting the right codes, or navigating denials, every step matters. With the right tools, knowledge, and in some cases, specialized support like ABA billing services, both patients and providers can experience a smoother, more transparent process.
Mental health care is about connection, healing, and growth. Clear and efficient billing ensures that nothing gets in the way of that journey.